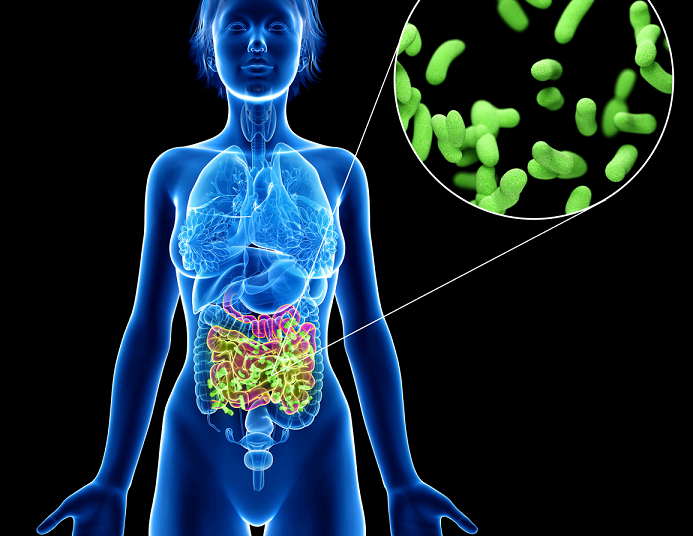
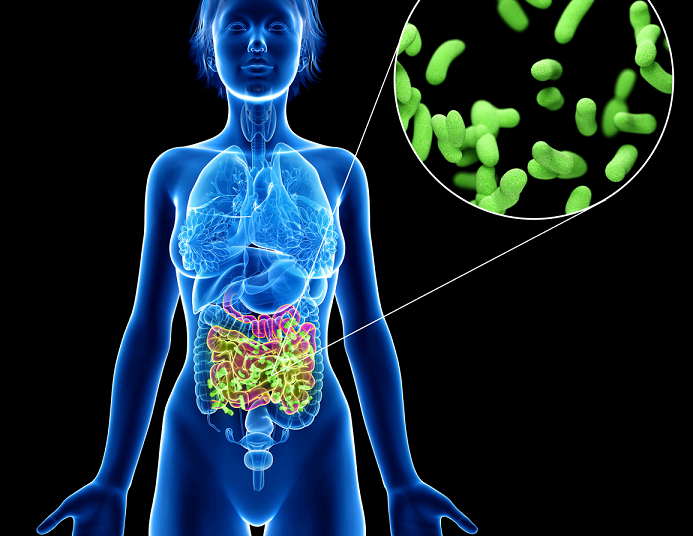
The relationship between our gut microbiome and various neurological diseases and chronic pain has received increasing attention. The gut microbiome is a crucial modulator of certain types of pain such as visceral pain. Recent evidence suggests that gut microbiota play a critical role in many other types of chronic pain, including inflammatory pain, headache, and neuropathic (nerve) pain.

How’s your gut health? A simple “gut check” is one of the most comprehensive ways to assess your overall well-being. Growing research points to the importance of the microbiome not only in pain but in a wide range of functions– from your immune system, to your weight, to your mental health and more.
The term microbiome refers to the trillions of microorganisms – bacteria, fungi, and other living microorganisms that exist in your gut. It’s a complex world, with hundreds of different kinds of bacteria. Those microorganisms are the foundation of the gut-brain axis, the two-way communication network between your brain and your gut.
Maintaining the microbiome requires a delicate balance of bacteria. The “good” bacteria helps digest food, absorbs nutrients, helps produce vitamins and hormones, and protects against “bad” bacteria. A myriad of factors can impact this balance. High-fiber foods are beneficial – gut bacteria break down fiber to digest it, a process which stimulates the production of more bacteria. A varied, nutrient-rich diet is important for a diverse biome, something that isn’t typically possible if you eat a lot of processed food. Stress, alcohol, and many medications may also alter the composition of the microbiome.
Is Your Gut Healthy? 5 Ways To Tell
Scientists are only just beginning to learn about the complexity of the microbiome. Despite the many mysteries still to discover, it’s actually quite easy to do a general check of your gut health. Following are some things to look for.
1 – Transit time
Healthy digestion is the key to maintaining the microbiome, and one indication of that is transit time, which is how long it takes food to pass through your digestive system. Why does this matter? Slower digestion can lead to the formation of harmful bacteria. On the other hand, when food passes through your body too quickly, you may not absorb essential nutrients. Although everyone is slightly different, optimal transit time is from 12 to 24 hours, which, for most of us, means one to two bowel movements a day. If you have no idea how long it takes to digest food, try eating about a half cup of raw beets, then keep an eye on the color of your stool.
How to improve transit time:
- Foods high in fiber keep things moving through your intestinal tract, so focus on unprocessed fruits and vegetables and whole grains.
- Many people find that dairy and overly processed foods slow digestion.
- Movement leads to increased blood flow and stimulates peristalsis, the wavelike contractions that move food through the intestines. Many yoga poses can help with digestion, particularly twisting moves.
- Some supplements that can speed up digestion include magnesium citrate and supplements with psyllium. However, it’s important to work with a healthcare practitioner to determine the correct use and dose. It’s possible to become dependent on supplements and laxatives, which can ultimately harm your digestive system.
2 – Perfect poops
It’s nobody’s favorite subject, but the condition of your poop actually gives a good indication of your intestinal health. The Bristol Stool Scale provides an easy visual reference. Some key things to look for include:
- Texture: Should be smooth. Hard, lumpy poops often indicate constipation.
- Shape: Sausage-shaped is ideal. Overly liquid is typically a sign of diarrhea, and pellet shapes are a sign of constipation.
- Buoyancy: Sinks in the toilet. Poop that floats may contain undigested fat.
Any straining or experiencing any pain during bowel movements should be investigated, as should any blood. Get to know your own body, and be alert to any changes.
3 – Gas after meals is not disruptive or painful
Some gas is inevitable after a meal, and some foods, like beans and raw veggies, certainly trigger gas more than others. Excess gas, however, can indicate something is amiss in your gut. While everyone has a different baseline, pay attention if you notice changes in your level of gassiness, or if gas causes distress or pain.
Easing gassiness
The following tips can reduce gassiness:
- Chew food slowly and thoroughly. The more you break down food in the mouth the easier it is to further digest.
- Keep a food diary to identify triggers. Common culprits include legumes and dairy products.
- Try a short walk after a large meal since movement helps stimulate peristalsis.
- Limit the consumption of carbonated drinks.
- Try probiotic supplements. It’s best to work with a healthcare practitioner, since sometimes excess probiotics can actually cause gas.
4 – Good energy levels
Do you feel rested when you wake up? The answer is a good indicator of your gut health. Since we get energy as food is digested, your gut health is essential to your energy level, and how ready you are to face the day. If you can’t break down food properly, you won’t receive vital essential nutrients. However, the role of your gut in fighting fatigue goes deeper than that. Bacteria in the microbiome impact our B vitamins, which are essential for energy. They also regulate the immune system, which is imperative for good energy.
5 – Your memory, mood, and focus
Growing research points to the impact of gut bacteria on our moods. Up to 90% of your body’s serotonin is produced in the gut, so it’s not surprising that altering the balance within the biome has notable effects on mood. Once again, this is a two-way street, as stress alters gut composition, which in turn can make you even more stressed because the gut’s production of hormones that impact your mood then shifts. It’s ultimately a sign of the importance of recognizing and addressing gut issues early.
The neurochemicals in your gut also impact your ability to learn new information and retain it. If you notice a change in your cognitive abilities, it’s a good idea to evaluate the other signs of a healthy gut to see if there is a connection.
How did your gut check turn out? If any items on this gut health checklist raise concerns for you, or you suffer from chronic pain and gut issues, don’t hesitate to reach out! At Revitalize Medical Center, we treat pain in a comprehensive, integrative approach to optimize wellness and health.
Disclaimer:
This website (including all pages and blog posts) is not intended to replace the services of a physician, nor does it constitute a doctor-patient relationship. Information is provided for informational purposes only and is not a substitute for professional medical advice. You should not use the information on this website for diagnosing or treating a medical or health condition. To schedule an appointment at Revitalize Medical Center, please call (847) 834-4018.
Reference:
- Guo R, Chen LH, Xing C, Liu T. Pain regulation by gut microbiota: molecular mechanisms and therapeutic potential. Br J Anaesth. 2019 Nov;123(5):637-654. doi: 10.1016/j.bja.2019.07.026. Epub 2019 Sep 21. PMID: 31551115.
- Madison, Annelise, and Janice K Kiecolt-Glaser. “Stress, depression, diet, and the gut microbiota: human-bacteria interactions at the core of psychoneuroimmunology and nutrition.” Current opinion in behavioral sciences vol. 28 (2019): 105-110. doi:10.1016/j.cobeha.2019.01.011
- John F. Cryan, Kenneth J. O’Riordan, Caitlin S. M. Cowan, Kiran V. Sandhu, The Microbiota-Gut-Brain Axis, Physiological Reviews, 28 AUG 2019, https://doi.org/10.1152/physrev.00018.2018
- Science Daily, “Food’s transit through the body is a key factor in digestive health,” June 27, 2016
- Li Y, Hao Y, Fan F, Zhang B. The Role of Microbiome in Insomnia, Circadian Disturbance and Depression. Front Psychiatry. 2018;9:669. Published 2018 Dec 5. doi:10.3389/fpsyt.2018.00669
- Rao SSC, Rehman A, Yu S, Andino NM. Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis. Clin Transl Gastroenterol. 2018;9(6):162. Published 2018 Jun 19. doi:10.1038/s41424-018-0030-7
- Holzer P, Farzi A. Neuropeptides and the microbiota-gut-brain axis. Adv Exp Med Biol. 2014;817:195-219. doi:10.1007/978-1-4939-0897-4_9
